Sickle Cell Anemia or Sickle Cell Disease: Know What It Is And How It Can Be Diagnosed And Treated
November 3, 2021
Sickle Cell Anemia, also known as Sickle Cell Disease, is a genetic disease
hereditary. Most people get the genes for hemoglobin called A from their father and mother. They are therefore called AA. But there are people who receive from their parents the genes for hemoglobin known as S, that is, they are SS. These people have the manifestations (symptoms) of Sickle Cell Disease.
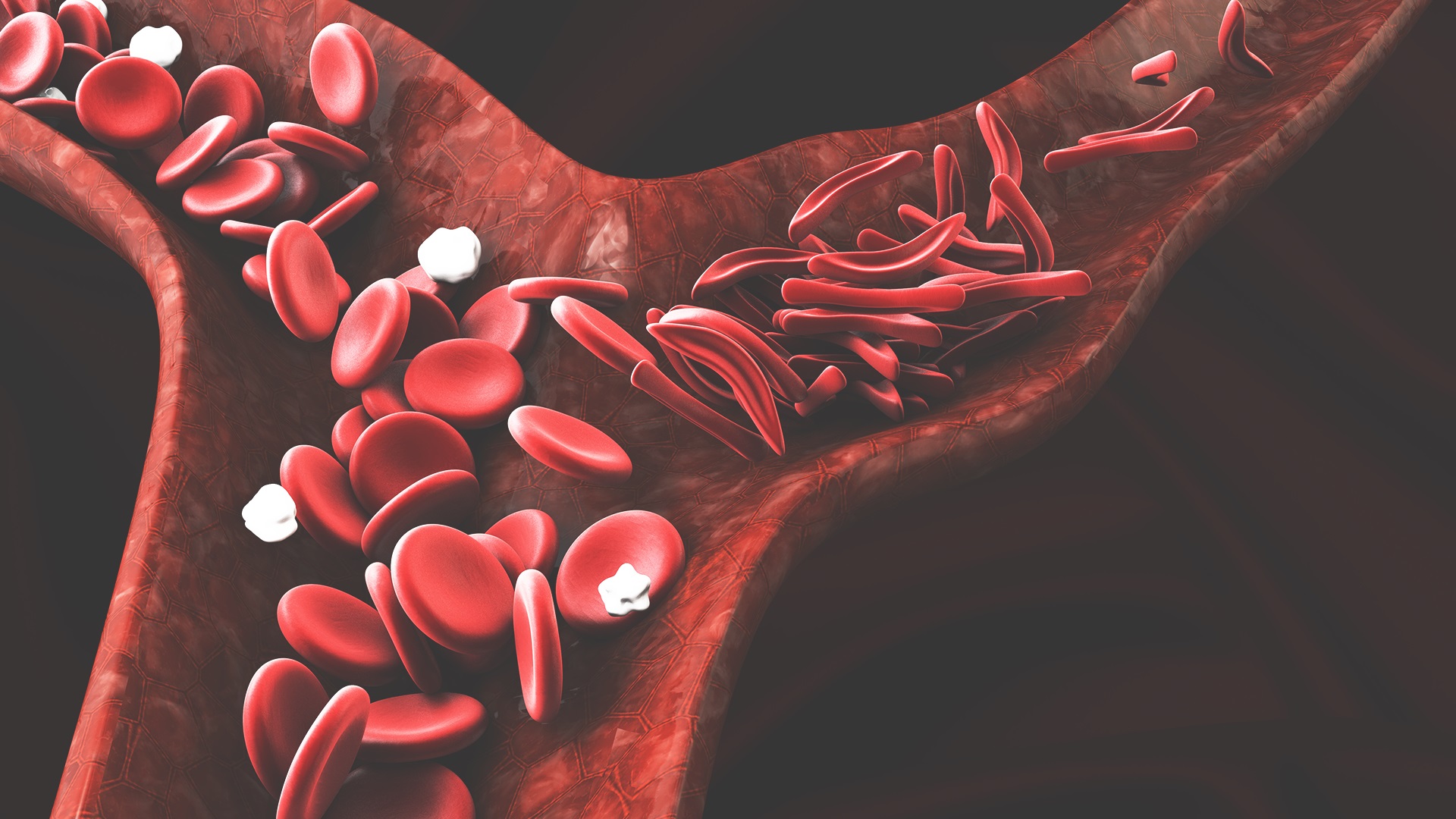
The disease is the result of a genetic mutation that causes changes in erythrocytes (red blood cells), present in the blood and essential for the transport of oxygen and carbon dioxide throughout the body. Under normal conditions these cells have a rounded shape. However, in the presence of Sickle Cell Disease they lose elasticity, stiffen and acquire a sickle shape, causing obstruction of blood flow and preventing the arrival of oxygen to the brain, lungs, kidneys and other organs and tissues of the body.1
Sickle cell disease is very common in black people, descendants of populations from North Africa and the Mediterranean, but in Brazil, due to the intense miscegenation that occurred in the country, it can also be observed in people of white or brown race.2
Sickle Cell Trait.
Sickle Cell Trait means that the person has inherited the gene for hemoglobin A from one parent and the gene for hemoglobin S from the other, that is, he is AS. People with Sickle Cell Trait are healthy and never develop the disease.
However, it is important to know that two people with Sickle Cell Trait can have children with Sickle Cell Anemia. Therefore, it is important that these people, regardless of their color or ethnicity, take the Hemoglobin Electrophoresis test before having a child.
DF: a public health problem.
For a long time, Sickle Cell Disease was an invisible disease. The first record was made in 1910, almost two centuries after the arrival of the first carriers of the genes that cause the disease to the American continent. Today, it is a serious public health problem, with an impact on the morbidity and mortality of the affected population, greatly impairing their quality of life, due to the severe pain it causes, with changes in the function of the kidneys, lungs and eyes, recurrent infections, neurological problems and iron overloads in the body, which lead to recurrent hospitalizations and reduced survival. Research shows that only 20% of children with sickle cell disease reach five years of age when they do not receive adequate and timely treatment.3
The fight against the disease, therefore, requires from governments an effective public health policy for the assistance and follow-up of patients who suffer from the disease.
Main symptoms of Sickle Cell Anemia.4,5,6
The symptoms of Sickle Cell Anemia appear in the first year of life and although they may manifest differently from individual to individual, the main signs of the disease are:
– Pain crisis: Pain in bones, muscles and joints due to vaso-occlusion with reduced flow of blood and oxygen to tissues and organs is the most common symptom of the disease.
- Pallor and tiredness: because of the reduction of circulating oxygen.
– Jaundice: yellowish color more visible in the sclera (whites of the eyes), due to the excess of bilirubin in the circulatory system, resulting from the rapid destruction of red blood cells.
– Hand-foot syndrome: attacks of pain in children's hands and feet, caused by swelling, pain and redness at the site, due to inflammation of the soft tissues that involve the joints of the wrists, ankles, fingers and toes.
– Infections: people with sickle cell disease are prone to infections, so children with this condition are more prone to pneumonia and meningitis.
– Delayed growth and sexual maturation: by the presence of anemia, infections and interference in hormone production.
– Leg ulcers, more frequent near the ankles: they usually start in adolescence and can become chronic due to blood viscosity and poor peripheral circulation. A wound can take years to heal if not cared for at first.
– Sequestration of blood in the spleen, known as splenic sequestration: in children with sickle cell anemia, the spleen can increase in size by retaining all the blood and quickly lead to death from lack of blood to other important organs in the body, such as the brain and heart. It therefore requires emergency treatment as it involves a serious risk to life.
It is worth remembering that Sickle Cell Anemia has no cure and can compromise the main functions of the body if the patient does not receive adequate care.
Neonatal diagnosis and treatment.
The best way to diagnose sickle cell disease early is the famous foot test, a neonatal screening performed free of charge in maternity hospitals through hemoglobin electrophoresis, a set of blood tests usually performed within the first 24 hours of a newborn's life. The sample is obtained by puncturing the calcaneus and collected on filter paper.
Once the disease is confirmed, the baby must have adequate medical follow-up for life, based on a comprehensive care program. The family plays a fundamental role in the treatment, and must pay close attention to the child's growth and development.4,6
Already in adulthood, the blood test is the key to the beginning of treatment, and late diagnosis can lead to death. The preventive examination can be done in the public network and is recommended for people between 2 and 17 years of age.
Overview of sickle cell disease in Brazil.
According to data from the Ministry of Health, between 25,000 to 50,000 people suffer from sickle cell disease in Brazil and around 3,500 new cases are detected each year.
The proportion of live births with sickle cell disease and trait in some Brazilian states has the following numbers: Bahia 1:650; Rio de Janeiro 1:1,300; Pernambuco, Maranhão, Minas Gerais and Goiás 1:1,400; Sao Paulo 1:4,000; Mato Grosso do Sul 1:5,850; Rio Grande do Sul 1:11,000.7
The Guidelines for the National Policy for Comprehensive Care for People with Sickle Cell Disease are defined by the National Policy for Comprehensive Care for the Health of the Black Population, of the Ministry of Health, and in the regulation of the Unified Health System (SUS).
Due to the high morbidity and mortality rate of the disease, in 2001 the MS included the detection of hemoglobinopathies in the National Neonatal Screening Program (PNTN), allowing diagnosis from the first week of life and benefiting patients early in care and treatment.8
Treatment alternatives offered by the SUS.
In 2005, within the scope of the Unified Health System (SUS), the National Policy for Comprehensive Care for People with Sickle Cell Disease (PNAIPDF) was instituted. It is an instrument to support states and municipalities in the implementation of health actions for the organization of the line of care and the inclusion of the theme in the Health Care Networks.
Currently, all Brazilian states have at least one specialized center to care for people with Sickle Cell Disease, who must be identified in a comprehensive family health care program.
Among the medicines distributed free of charge at the Basic Health Units (UBS), there are folic acid, analgesics, anti-inflammatories, iron chelators, special immunobiologicals and antibiotic therapy. The Transcranial Doppler preventive exam is also available, which identifies the risk of stroke in people with Sickle Cell Disease, between 2 and 16 years old.9
In addition to diagnosis and medication, the Unified Health System also offers treatment options free of charge, including bone marrow transplantation (BMT), in the case of patients who meet certain prerequisites.
References:
- Gov.br – Ministry of Health. Ministry of Health reinforces the importance of detecting sickle cell disease. Available in: https://www.gov.br/saude/pt-br/assuntos/noticias/ministerio-da-saude-reforca-a-importancia-da-deteccao-da-doenca-falciforme Accessed in October 2021.
- Sickle cell anemia: trait, signs and treatment. Available in: https://www.mdsaude.com/hematologia/anemia-falciforme Accessed in October 2021.
- Brazilian Society of Tropical Medicine. Almost half of Brazilians are unaware of the most prevalent hereditary disease in the country, according to unprecedented research. Available in: http://www.sbmt.org.br/portal/quase-metade-dos-brasileiros-desconhece-doenca-hereditaria-de-maior-prevalencia-no-pais-aponta-pesquisa-inedita/?locale=pt-BR Accessed in October 2021.
- Ministry of Health. Virtual Health Library. Available in: https://bvsms.saude.gov.br/19-6-dia-mundial-de-conscientizacao-sobre-a-doenca-falciforme/ Accessed in October 2021.
- Ministry of Health. Virtual Health Library. Available in: https://bvsms.saude.gov.br/anemia-falciforme Accessed in October 2021.
- AAFESP – Association of Sickle Cell Anemia of the State of São Paulo. Sickle Cell Anemia. Available in: https://aafesp.org.br/index.php/anemia-falciforme Accessed in October 2021.
- Ministry of Health. Federal government. Sickle cell disease. Available in: https://bvsms.saude.gov.br/bvs/folder/doenca_falciforme_flyer_web.pdf Accessed in October 2021.
- Sickle cell disease. Available in: https://sp.unifesp.br/epe/desc/noticias/doenca-falciforme Accessed in October 2021.
- Health Channel. Treatment for sickle cell disease is available from SUS. Available in: https://www.canalsaude.fiocruz.br/noticias/noticiaAberta/tratamento-para-doenca-falciforme-esta-disponivel-no-sus19062019 Accessed in October 2021.